Mature B-cell neoplasms
(Overview)
- Method:
- Anticoagulant:
- Recommendation:
- Method:Cytomorphology
- Anticoagulant:EDTA
- Recommendation:obligatory
- Method:Immunophenotyping
- Anticoagulant:EDTA or Heparin
- Recommendation:obligatory
- Method:Chromosome analysis
- Anticoagulant:Heparin
- Recommendation:facultative
- Method:FISH
- Anticoagulant:EDTA or Heparin
- Recommendation:obligatory
- Method:Molecular genetics
- Anticoagulant:EDTA or Heparin
- Recommendation:entity specific
Based on the current guidelines and the current state of research, there are different diagnostic recommendations for patients with mature B-cell neoplasms. We have summarized the most important information about the classification and diagnostic methods at MLL. In addition, we provide further links to the various diseases.
Mature B-cell neoplasms: General overview
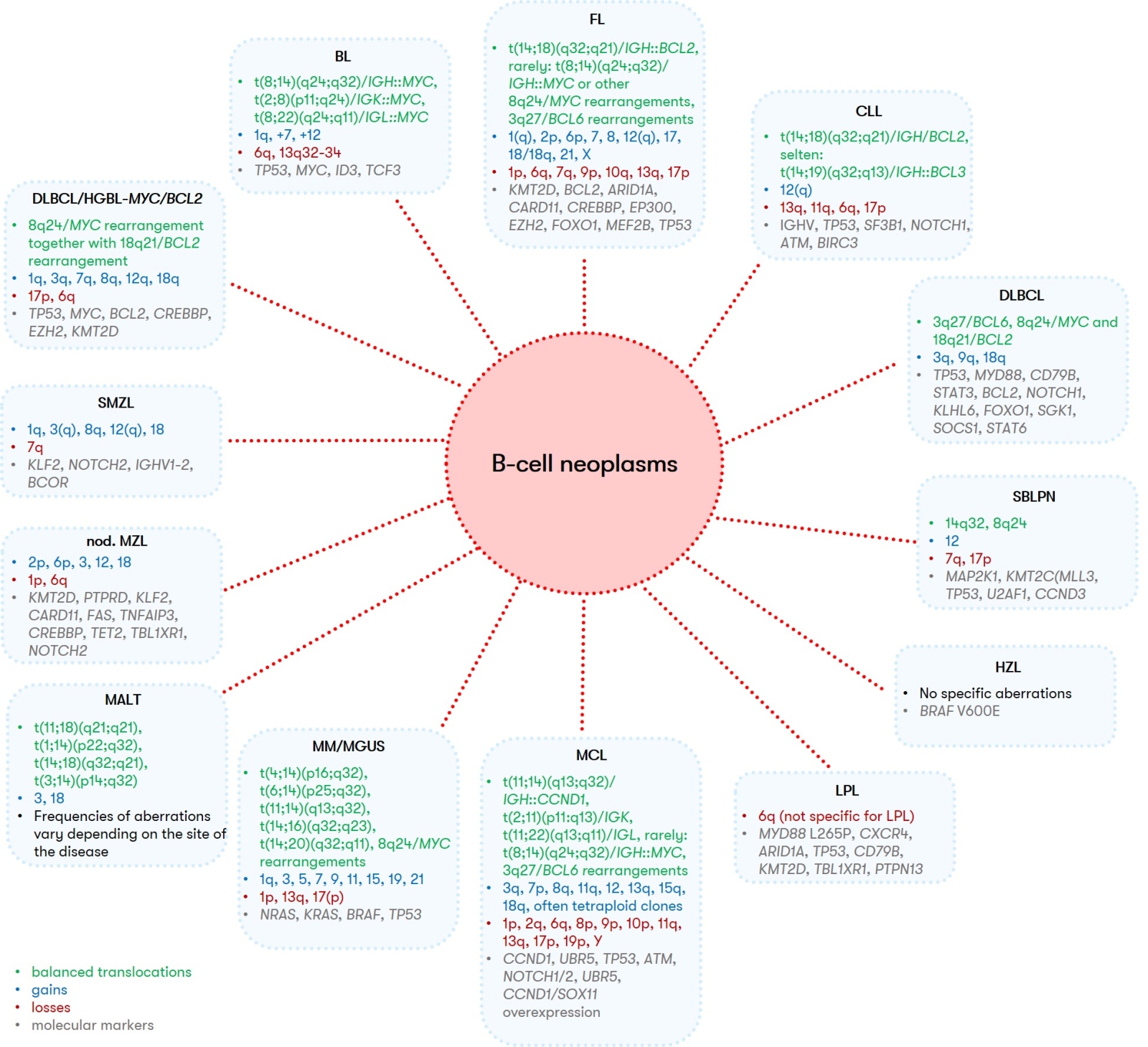
Mature B-cell neoplasms are biologically and clinically highly heterogeneous diseases of the B-lymphatic system. Depending on the entity, the clinical courses range from indolent to aggressive. Based on histology and immunophenotype, the WHO classification describes 47 different entities of mature B-cell neoplasms (WHO 2022). These exhibit a broad spectrum of possible genetic aberrations, partly showing typical patterns of balanced and/or unbalanced aberrations, which are, however, not specific enough for a definitive diagnosis. In the following overview, the characteristic immunophenotypic (cf. Table 1) and genetic features (cf. Fig. 1) of mature B-cell neoplasms are presented, which, in combination with the methods of histology, immunohistochemistry and cytomorphology, allow an exact diagnostic classification.
MLL provides additional information on the following entities:
- Burkitt’s lymphoma (BL)
- Chronic lymphocytic leukemia (CLL)
- Diffuse large B-cell lymphoma (DLBCL)
- Follicular Lymphoma (FL)
- Hairy cell leukemia (HZL)
- Splenic B-cell Lymphoma/Leukemia with prominent nucleoli (SBLPN)
- High grade B-cell lymphoma (HGBL)
- Lymphoplasmacytic lymphoma (LPL)/Waldenström macroglobulinaemia
- Mantle Cell Lymphoma (MCL)
- Splenic marginal zone lymphoma (MZL)
- Monoclonal B-cell lymphocytosis (MBL)
- Multiple myeloma (Plasma Cell Myeloma) & monoclonal gammopathy of undetermined significance (MGUS)
Mature B-cell neoplasms: Diagnostic methods
Diagnostics is based on the interaction of different methods:
- Cytomorphology: Assessment of the degree of maturation and infiltration in bone marrow and peripheral blood, respectively.
- Immunophenotyping: Assignment to the B- or T-cell lineage. Many lymphoid entities show characteristic immunophenotypes (e.g. FL or MCL), these are summarized in Table 1.
- Chromosome analysis, FISH, Molecular genetics: Detection of characteristic genetic aberrations, an overview is provided in Fig. 1.
- Immunohistochemistry: Central role in the context of histopathology, especially of the lymph nodes.
Mature B-cell neoplasms: Prognosis
Due to the heterogeneity and complexity of the aberration spectrum, the prognostic significance in individual cases is highly variable within the different entities. In addition to clinical parameters, many individual diagnostic findings are of decisive importance for the right timing between watch and wait and therapy initiation. Increasingly, these findings also directly influence the choice of therapeutic agents (precision medicine) and are taken into account in the approval of drugs (e.g. TP53 alterations in CLL).
Mature B-cell neoplasms: Recommendation
The diagnosis of mature B-cell neoplasms is now much more comprehensive than it was 5-10 years ago and in many cases their results from blood, bone marrow and/or lymph nodes have a direct impact on the choice of a potential therapy in addition to diagnostic and prognostic relevance. Various therapeutic approaches are so effective that today the determination of measurable residual disease (MRD) is in part included in remission controls. The method of choice is usually immunophenotyping.
Important note on the test material
If lymphoma cells are detected in the peripheral blood, the diagnosis can initially be made with a high degree of certainty without a bone marrow biopsy or lymph node sampling. Based on these findings, an extended material sampling is useful in individual cases and if clinically relevant.
Status: August 2023