Clonal hematopoiesis risk score
The molecular genetic detection of clonal hematopoiesis by sequencing allows us to better understand the early phase of the development of myeloid neoplasms. The prevalence of clonal hematopoiesis is strongly age-dependent, ranging from 10-20% of the population over 60 years of age, so we are increasingly confronted with this question in the workup of blood count abnormalities. The WHO classification 2022 distinguishes clonal hematopoiesis of indeterminate potential (CHIP) and clonal cytopenia of indeterminate significance (CCUS) as myeloid precursor lesions. The risk of progression from clonal hematopoiesis to full-blown myeloid neoplasia depends on the number and type of underlying mutations and clone size. In addition, the presence of unexplained hematopoietic changes, especially unexplained cytopenia (i.e., diagnosis of CCUS rather than CHIP), is the major risk factor for hematologic progression. However, no generally accepted prognostic models have been available to accurately predict individual risk.
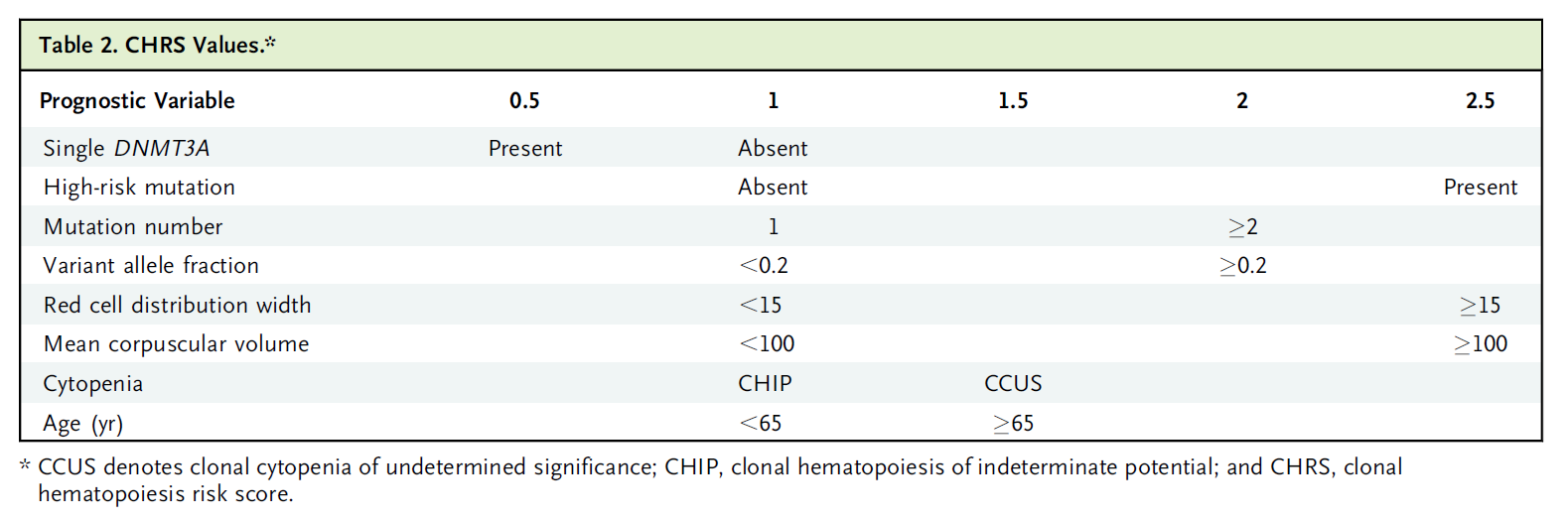
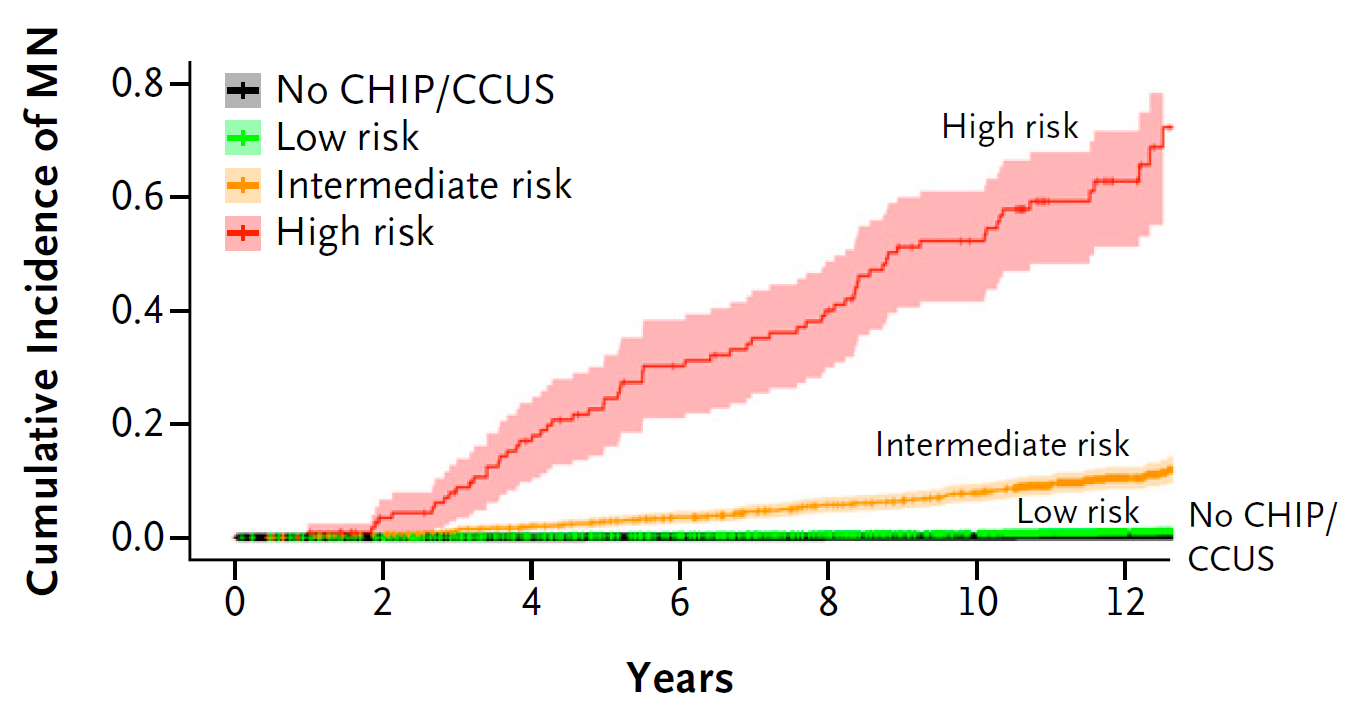
In a recently published study (Weeks LD et al, NEJM Evid 2023;2(5)), the risk of progression of clonal hematopoiesis was investigated in a large cohort of 438,890 subjects from the U.K. Biobank and a Clonal Hematopoiesis Risk Score (CHRS) was established. Prognostically unfavorable variables included defined high-risk mutations (SRSF2, SF3B1, ZRSR2, IDH1, IDH2, FLT3, RUNX1, JAK2, and TP53), detection of multiple mutations, a clone size of at least 20% variant allele frequency (VAF), a red cell distribution width (RDW) of ≥15%, macrocytosis defined as mean red cell volume (MCV) of ≥100 fl, the presence of cytopenia (CCUS vs. CHIP) and an age ≥65 years. In contrast, the presence of a DNMT3A mutation alone is a prognostically favorable factor in CHRS. The weighted sum of these factors results in a CHRS score, on the basis of which individuals with clonal hematopoiesis are classified into the risk categories of low (score ≤9.5), intermediate (score 10-12), and high (score ≥12.5). For individuals in the lowest risk category (approximately 90% of all individuals with clonal hematopoiesis), the 10-year risk of developing a hematologic neoplasm was <1% and thus only marginally increased compared with individuals without clonal hematopoiesis. In contrast, the 10-year progression rates in the intermediate (approximately 10% of all individuals with clonal hematopoiesis) and high risk categories (approximately 1% of all individuals with clonal hematopoiesis) were 8% and 52%, respectively, in a clinically relevant range, which was also reflected accordingly in overall survival.
The CHRS risk score for clonal hematopoiesis allows improved prediction of progression risk in individuals with CHIP and CCUS based on simple blood count variables and molecular genetic NGS examination of a myeloid gene panel. While the corresponding analyses can in principle be performed in peripheral blood, the combination of an unclear cytopenia and the detection of a somatic mutation still indicates a bone marrow biopsy to clarify the presence of an already manifest myelodysplastic neoplasia (MDS) or other hematologic neoplasia.
Table: CHRS values (Weeks et al. 2023).
References
Weeks LD et al. Prediction of risk for myeloid malignancy in clonal hematopoiesis. NEJM Evid 2023;2(5).

«Do you have questions about the article? Please feel free to send me an e-mail»
PD Dr. med. Gregor Hörmann, PhD