More precise relapse prognosis for CML patients: Cell line-specific detection in measurable residual disease
- New horizons in leukemia research: Selected papers in focus -
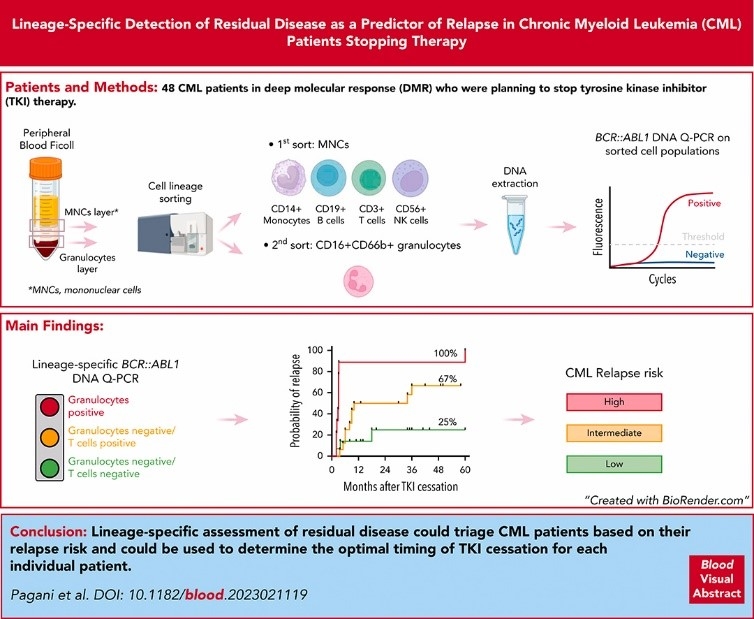
A new study by Pagani et al. examines the role of cell line-specific measurement of BCR::ABL1 transcripts by quantitative PCR in different immune cell populations with a view to more precise methods for predicting relapse after the end of therapy. According to the study, the detection of BCR::ABL1 DNA in granulocytes and T cells after discontinuation of therapy could be a better predictor of relapse than detection in total leukocytes.
Patients with chronic myeloid leukemia (CML) who are eligible for treatment-free remission (TFR) may relapse even after discontinuation of a tyrosine kinase inhibitor (TKI). There is therefore a need for precise predictors - such as the sensitive detection of measurable residual disease (MRD). However, this evidence can vary in its significance: According to the authors of the publication presented here, this could be due to the fact that MRD measures the total leukocyte count, although only certain cell types are relevant for recurrence. In their prospective study, Pagani et al. therefore investigated whether the measurement of BCR::ABL1 transcript levels in different immune cell populations (granulocytes, T cells, NK cells, B cells and monocytes) using quantitative real-time PCR (qPCR) can predict the risk of relapse after discontinuation of TKI therapy in patients with CML. For this purpose, 47 CML patients who planned to discontinue TKI therapy were analyzed and followed up for up to five years. 40 of these patients, who were attempting to achieve a TFR for the first time, were selected for subsequent predictive analyses.
Detection of BCR::ABL1 DNA was associated with a higher cumulative incidence of relapse at 60 months (70% vs. 30%; P=0.023) in total leukocytes. The highest transcript level was detected in granulocytes (100% vs. 49%; P<0.0001), followed by T cells (73% vs. 30%; P=0.022). Using multivariate analysis, Pagani et al. were able to define three patient groups: Granulocyte-positive, granulocyte-negative/T-cell-positive and granulocyte-negative/T-cell-negative with a high, intermediate and low risk of recurrence, respectively. The accuracy of this model was 77%.
The authors assume that cell line-specific MRD measurement can be used to identify patients who can safely discontinue TKI therapy. In addition, the optimal time for ending therapy can be found. Pagani et al. also conclude that the detection of BCR::ABL1 DNA in granulocytes and T cells upon discontinuation of the TKI is a better predictor of relapse than detection in total leukocytes.
Pagani IS et al. Lineage-specific detection of residual disease predicts relapse in patients with chronic myeloid leukemia stopping therapy. Blood 2023;142(25):2192-2197.

"If you have any questions about these topics and the assessment of the MLL, please contact us!"
Dr. rer. nat. Constanze Kühn
Medical Writer