Diagnostic potential of immunophenotypic aberrations in MDS
The diagnosis of myelodysplastic neoplasms (MDS) and their classification into subgroups was based on cytomorphological features for a long time. Cytomorphology still plays a major role today, but cytogenetic criteria were added to the diagnostic criteria after the introduction of the WHO classification of tumors of hematopoietic and lymphoid tissue. It is now known that integrated diagnostics, including immunophenotyping and molecular genetics, are of great importance.
Immunophenotyping can be used to detect aberrant antigen expression patterns in suspected or confirmed MDS. This provides valuable information for diagnosis and prognosis. In a recent prospective and multicenter study, the International MDS-Flow (iMDS-Flow) working group of the European LeukemiaNet (ELN) validated the significance of different immunophenotypic markers and also identified important parameters that contribute to the clinical utility of immunophenotyping in MDS diagnostics (Kern et al. Cytometry B Clin Cytom 2022).
Immunophenotypic detection of MDS depends on a combination of MDS-associated aberrations and, to date, no flow cytometric score has been able to establish itself as the gold standard. The study described here has now identified 17 different immunophenotypic parameters independently associated with MDS or CMML in at least one of the subgroups (low-risk MDS, high-risk MDS, CMML) or the overall cohort. In addition, using a cut-off value of three independently occurring MDS/CMML-related aberrations, flow cytometric results showed a concordance of more than 80% with cytomorphology, regardless of the number of cell compartments affected. In high-risk MDS patients, the agreement was even above 90%.
Furthermore, the percentage of myeloid progenitor cells (MPCs) was identified as a strong indicator for MDS, correlating with disease risk. A cut-off of >3% MPCs detected by flow cytometry was strongly associated with MDS/CMML (98% of cases with more than 3% MPCs had MDS by cytomorphology) and can therefore be used - analogous to the value of 5% blasts in cytomorphology - in the diagnostic decision.
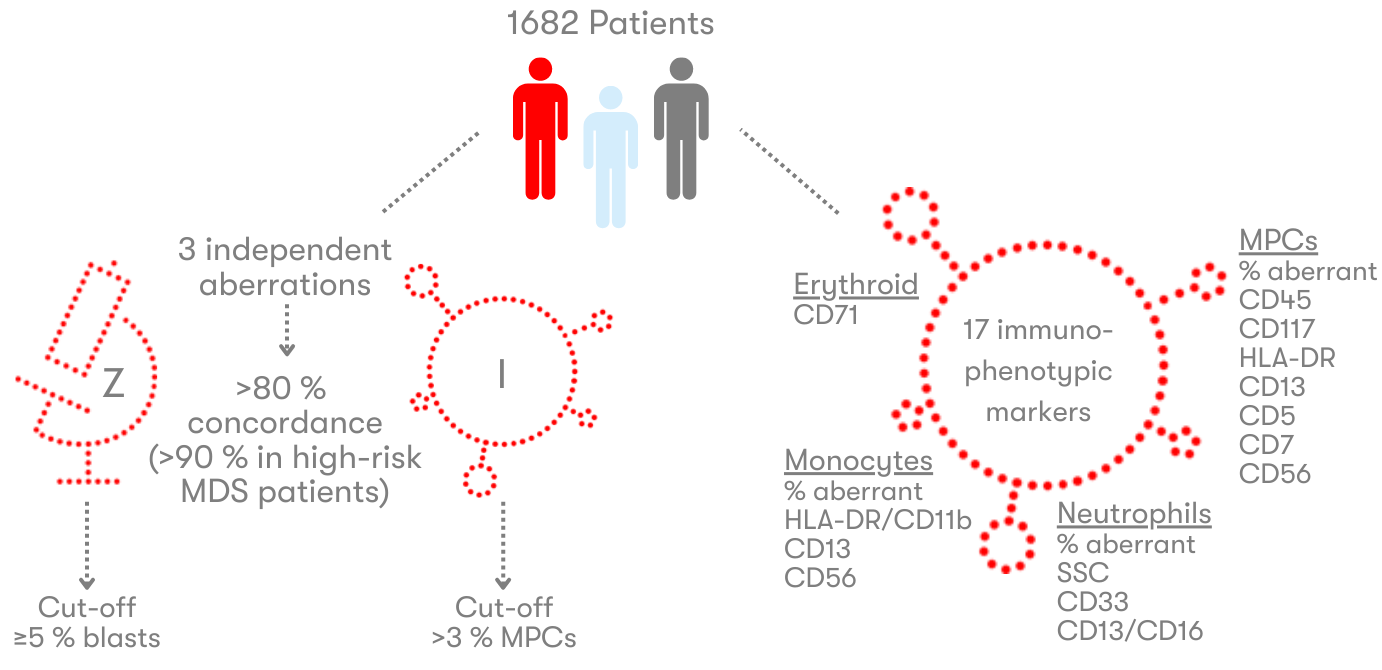
The iMDS Flow Working Group proposes that the 17 identified parameters should be mandatorily incorporated into routine diagnostics as a core set of markers for immunophenotypic evaluation of suspected MDS cases. Wherever possible, additional markers should be investigated, as listed in the ELN recommendations. This will ensure the most comprehensive evaluation possible. The high concordance of immunophenotyping and cytomorphology results across risk groups and subgroups also demonstrates the importance of an integrated diagnostic approach.
References:
Kern W et al. Multicenter prospective evaluation of diagnostic potential of flow cytometric aberrancies in myelodysplastic syndromes by the ELN iMDS flow working group. Cytometry B Clin Cytom 2023;104(1):51-65.
The author

»Do you have any questions about the item or would you like more information? Feel free to send me an e-mail.«
Prof. Dr. med. Wolfgang Kern
Executive Management
Internist, Hematologist and Oncologist
Deputy Head of Immunophenotyping
wolfgang.kern@mll.com